Fuel Your Prospective Care Programs with Advanced Analytics
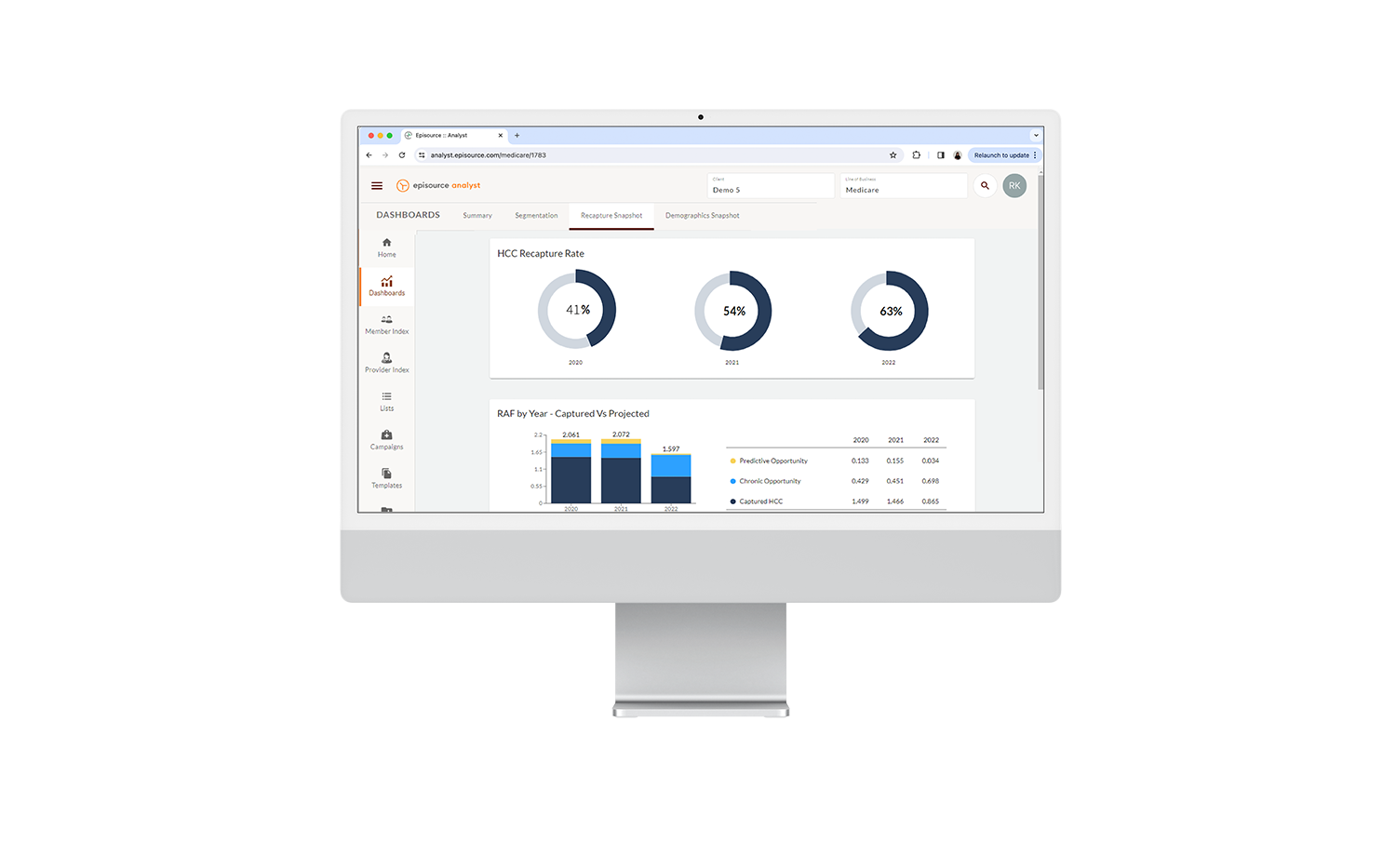
Episource Analyst is more than an analytics tool. It’s a comprehensive risk-adjustment analytics workflow platform that turns data into actionable insights at the touch of a button.
With Analyst, Medicaid health plans can launch and track campaigns to close risk score gaps, execute targeted interventions, and improve quality of care for your members — all within a single application.
Key Features
Risk Adjustment Suspecting
Leverage risk adjustment suspecting and gap analytics based on historical data with simple workflows to manage prospective, concurrent, and retrospective campaigns.
Streamlined UI
Customize your member- and provider-level reports and easily view campaign performance metrics, such as total eligible members and top 5 suspected and captured HCCs with our intuitive UI.
SDOH Analysis
Create member cohorts based on social determinants of health (SDOH) factors, including age, gender, zip code, race, and ethnicity. Then, leverage this analysis to identify which member segments need additional care or services.
Chase Lists
Generate chase lists by prioritizing high-risk members for more immediate care.
Member & Provider Stratification
Stratify members and providers by numerous data points and attributes, including risk scores, disease gaps, prevalence, eligibility, provider types, and more for direct, targeted impact at campaign or program levels.
Prospectively identify and close CDPS gaps
Generate provider education and partnership strategies
Support member engagement programs
Drive primary and specialty care by analyzing gaps
Support case management for high-risk members
Leverage member stratification to maximize program impact
Our Impact
"...When you establish a new relationship, you set some expectations, and some are lacking, some just meet expectations, and then you have that one or two who will exceed expectations — and that is Episource for us."
Episource Client
"You guys have put thought into things and understand risk. It's not just risk scores, it is so much more."
Episource Client
"Seeing the impact that we have on our providers has made it all worth it."
Episource Client
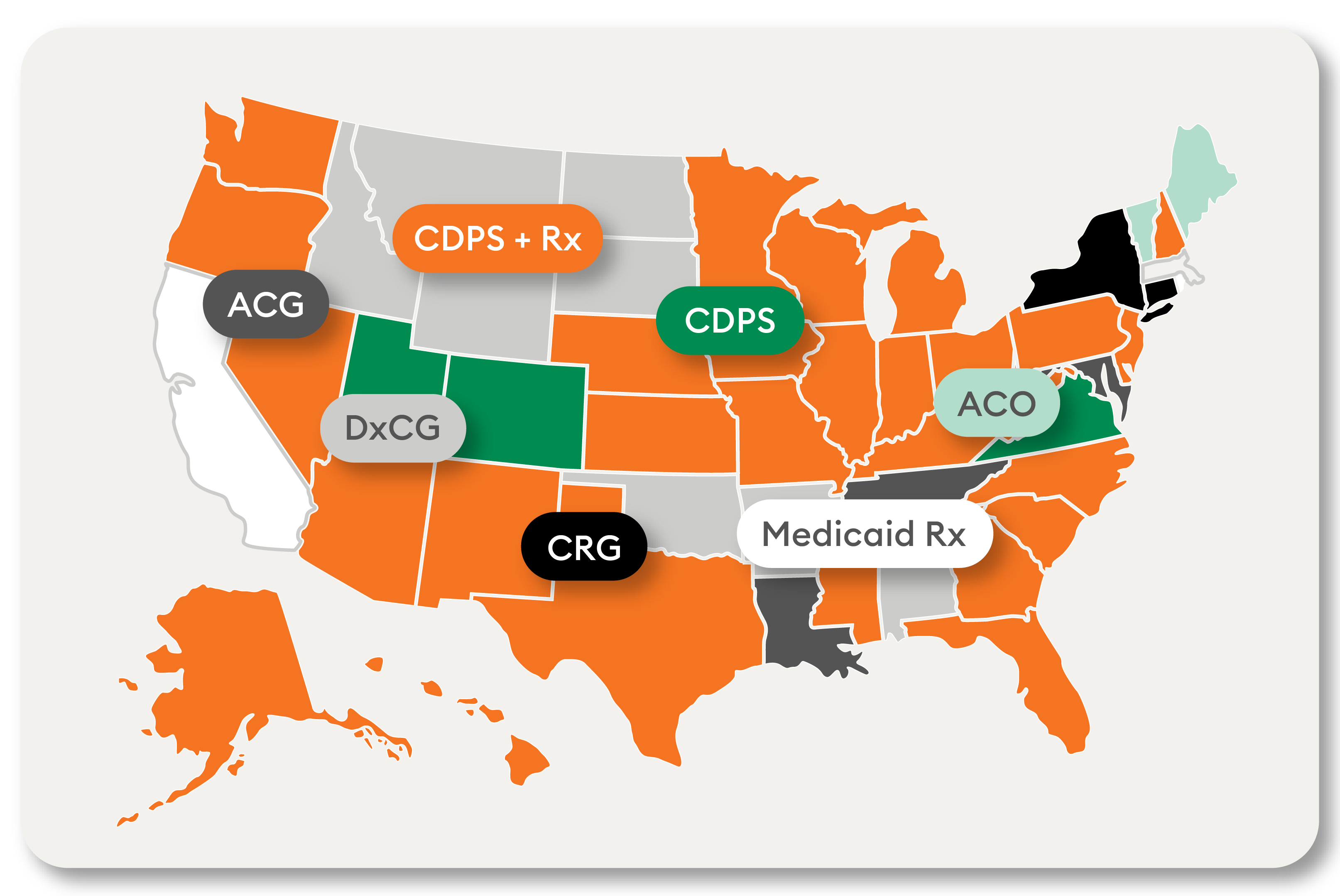
Master Medicaid Complexities with Advanced Analytics
We innovate for all health plans operating under the CDPS + Rx, CDPS, and Medicaid Rx models and handle all state-level definitions and complexities.
We also offer coding and submissions services to help you confidently submit accurate claims before CMS deadlines.
Additional Resources
Stay ahead with cutting-edge industry insights! Subscribe to our monthly newsletter today.
From Data to Strategy: Three Storytelling Tactics to Accelerate Data-Driven Decision Making in Healthcare Organizations
Approximately 30% of the world’s data volume today is being generated by the healthcare industry, yet only 20% of healthcare organization executives trust their data. While numerous healthcare organizations quote data quality, integration, and interoperability as their top strategic priorities, few prioritize programs focused on data literacy — the ability to think critically about data and to communicate data in a business context.
Streamlining Healthcare Coding and Enhancing Revenue Forecasting in the Face of the CMS-HCC V28 Model Transition
Shortly after the version 28 of the Hierarchical Condition Category (HCC) model was announced, Episource engaged with a diverse group of small- to medium-sized health plan clients facing the challenge of transitioning to the newly blended V24-V28 model.
Transitioning to V28 of CMS’ HCC Model: No Time Like the Present
On March 31, 2023, Centers for Medicare & Medicaid Services (CMS) announced the gradual transition to V28 of the CMS-HCC model. Phased in over time, the plan is to switch completely to the updated model by 2025. This change has widespread implications and all health plans should already be thinking about this transition.